Ocular surface and corneal diseases:
Keratoconus, Iritis and Pterygium
Ocular surface and corneal diseases, such as keratoconus, iritis and pterygium, all affect our eyes in different ways. Keratoconus- can affect the eye’s refractive ability and accelerate the progression of astigmatism. Corneal collagen cross‑linking strengthens the cornea by binding the collagen fibers more tightly together, providing treatment for keratoconus.Iritis, a viral or bacterial infection of the anterior part of the uvea, could lead to complications such as cataract, glaucoma and other complications. And Pterygium is a benign conjunctival lesion, a triangular wing-shaped foreign body that covers the white of the eye and extends to the cornea. When the pterygium gradually grows toward the pupil, it may become inflamed and cause the white of the eye to become red and swollen.It is a benign conjunctival growth, appearing as a triangular, wing‑shaped tissue that spreads over the white of the eye and extends to the cornea. When the pterygium gradually grows toward the pupil, it may become inflamed, causing redness and swelling of the eye. If these symptoms occur, please contact our center promptly to arrange diagnosis and treatment.
Keratoconus
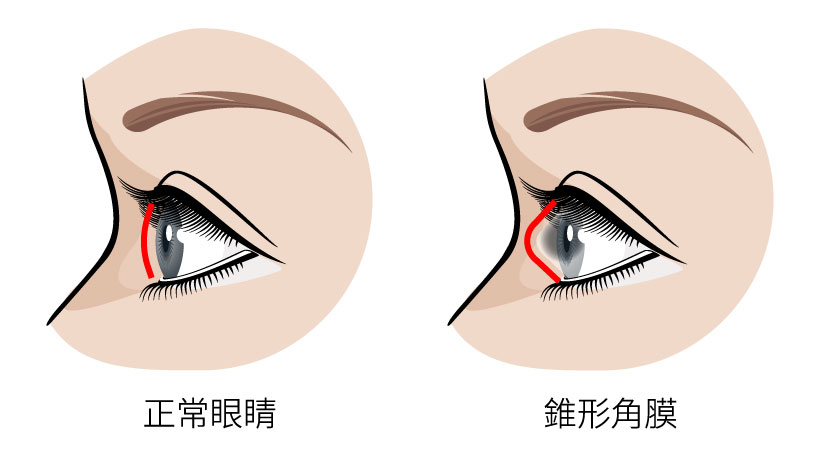
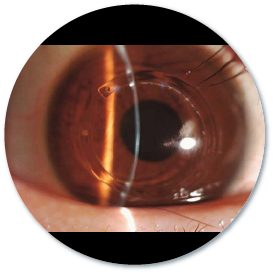
Also known as keratoconus, this condition occurs when the central cornea becomes thin and is pushed outward by intraocular pressure, altering its normal curvature and causing the cornea to bulge into a cone‑like shape. Keratoconus can impair the eye’s refractive ability and accelerate the progression of astigmatism. The exact cause is still unclear, but it may be related to frequent eye rubbing, allergic diseases, or genetic factors. Symptoms usually appear during puberty or in the twenties. Since early keratoconus resembles common astigmatism or myopia, patients may not realize they have a problem or seek medical advice, making diagnosis more difficult. As the condition progresses, vision may suddenly deteriorate, and even after treatment, corneal scarring can lead to permanent visual impairment.
Symptoms of Keratoconus
Bulging outward of cornea

Worsening in a greater and faster manner in myopia or astigmatism
Decreased visual function

Management of Keratoconus
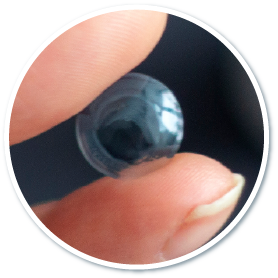
Hard contact lens
Hard contact lenses exert greater pressure on the top, so they can press the cornea to deform. However, they are less comfortable and may be displaced on the surface of the eyes.
Corneal collagen cross-linking
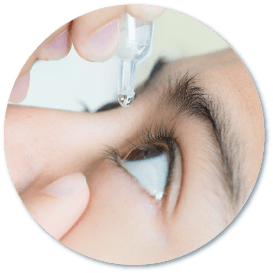
Corneal collagen cross-linking (also called corneal cross-linking ) is to apply riboflavin (a type of vitamin B2) eye solution to the patient's eyes, and then illuminate the eyes with ultraviolet light for 45 minutes to tighten the collagen in the corneal fibers, strengthening the cornea and making it stronger and more stable. This corneal cross-linking reduces the chance of corneal ectasia, deformation and degree rebound.
Precautions after corneal collagen cross-linking
- Avoid eye makeup
- Avoid getting shampoo or soap into your eyes
- Avoid getting perfume or hair spray into your eyes
- Do not drive until your vision is stable
- No swimming or steam bathing
- Avoid strenuous exercise, such as health dance and ball games
- Avoid drinking alcohol and smoking to avoid eye irritation
- Wear sunglasses when going out to prevent dust or foreign objects from entering your eyes
- Avoid places with turbid air
- Follow the doctor's instructions to instill eye drops and follow up regularly.
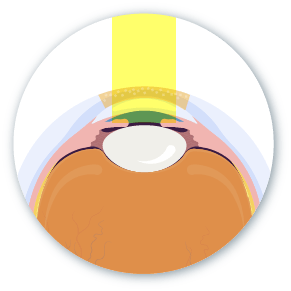
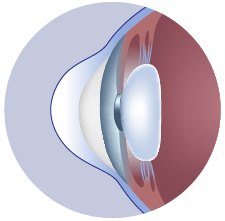
Implantation of Intra-Corneal Ring
Intra-Corneal Ring are two crescent-shaped pieces of a plastic that are implanted into the cornea stroma after a tiny incision is made in the cornea. Such procedure is to support the thin and weak cornea and flatten the central curvature of the cornea, which reduces irregular astigmatism and improves visual function. If postoperative vision improvement is not satisfactory, the Intra-Corneal Ring can be replaced or removed.
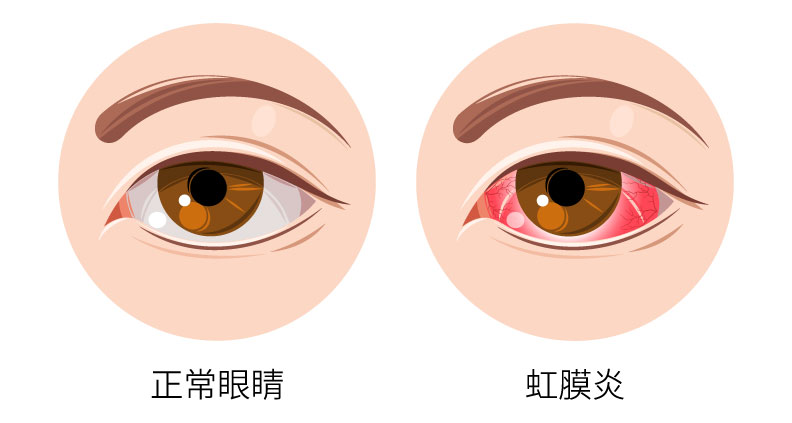
Iritis
The iris is the muscular tissue located between the cornea and the lens. It controls the size of the pupil and forms the front part of the uvea. Therefore, iritis refers to infection of the anterior uvea caused by viruses or bacteria. When the immune system malfunctions and attacks the iris cells, inflammation can also occur, leading to redness of the eye. Without timely treatment, complications such as cataracts or glaucoma may develop. Patients may need oral steroids or anti‑inflammatory eye drops to reduce redness and swelling and relieve eye pain. People often confuse iritis withConjunctivitis. It is often confused with conjunctivitis. However, iritis refers to inflammation inside the eye (the iris), while conjunctivitis refers to inflammation on the surface of the eye (the conjunctiva). Continue reading to learn more about the causes, symptoms, examinations, and management of conjunctivitis.
Symptoms of Iritis

Blurry vision
Sensitivity to light
(photophobia)
Eye pain
Red and itchy eyes

Eye floaters

Watery eyes

Steroid drugs
Management of Iritis
Mild cases
Patients can use steroid eye drops or ointment to control the condition
Severe cases

Patients need direct injection of medication into the eye to control inflammation. Some patients even have to take steroids to cure the condition fully.
Caution
Long-term application of steroids may increase the risk of cataracts and elevated intraocular pressure, so such medications must be prescribed by and under the supervision of an ophthalmologist and should not be purchased on your own.
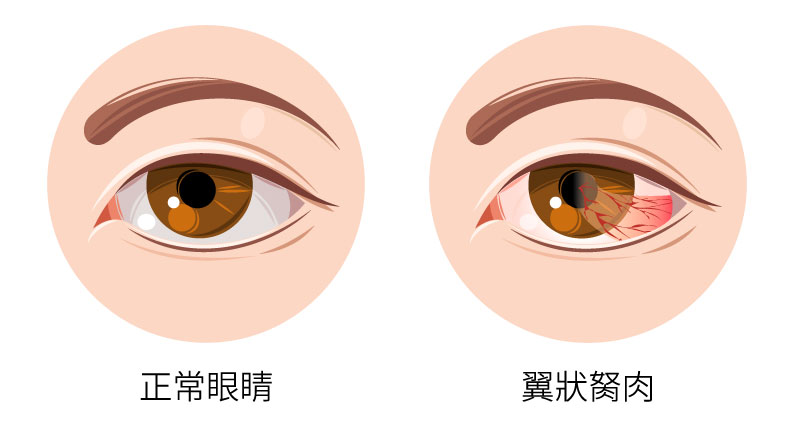
Pterygium is a benign conjunctival lesion, a triangular wing-shaped foreign body that covers the white of the eye and extends to the cornea. When the pterygium gradually grows toward the pupil, it may become inflamed and cause the white of the eye to become red and swollen.
Pterygium is a benign wedge-shaped fibrovascular growth of the conjunctiva that can enlarge and extend onto the cornea. As the pterygium grows into the pupil, it may become inflamed and cause redness and swelling in the white of the eye. The exact cause of the disease is uncertain. However, prolonged exposure to sunlight or UV light, and irritants like sand and wind will increase the risk of vascular tissue proliferation and increase the chance of pterygium enlargement.
Symptoms of Pterygium
Red and itchy eyes
Foreign body sensation

Visual impairment

Burning sensation & inflammation

Some patients have no symptoms

Management of Pterygium
Pterygium removal
Until now, there is no medicine that can effectively stop the growth of pterygium, and removal is the only way.
Artificial tears
Artificial tears can moisturise the cornea to relieve dry eyes, control minor symptoms and prevent inflammation.