


Dry Eye
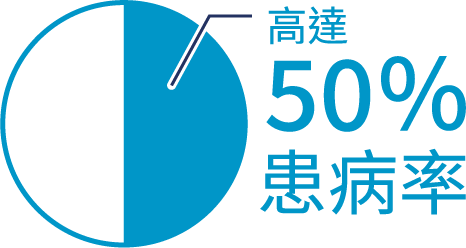
Dry eye syndrome (also known as dry eye disease) is one of the most common eye conditions worldwide. According to a study published in the Global Health Journal¹, the prevalence of dry eye can be as high as 50% globally. Causes of dry eye include prolonged use of digital devices, wearing contact lenses, aging, hormonal changes, certain medications, and environmental factors. If persistent symptoms such as dryness, itching, or light sensitivity are left untreated, they may cause corneal abrasion, inflammation, or ulceration, resulting in deteriorating vision, and in severe cases, even blindness. At the CUHK Medical Dry Eye Centre, our ophthalmologists provide examinations and treatments such as IPL (intense pulsed light therapy) and the iTEAR device to stimulate natural tear production.
Source: 1. Ophthalmology and Visual Sciences, The Chinese University of Hong Kong
Source: 1. Ophthalmology and Visual Sciences, The Chinese University of Hong Kong
Dry eyes are caused when the eye does not produce enough tears or when the tears evaporate excessively, resulting in the surface of the eye not remaining moist and hence feeling dry.
The tear layer on the surface of the eyeball is divided into three layers: oil layer, aqueous layer, and mucus layer
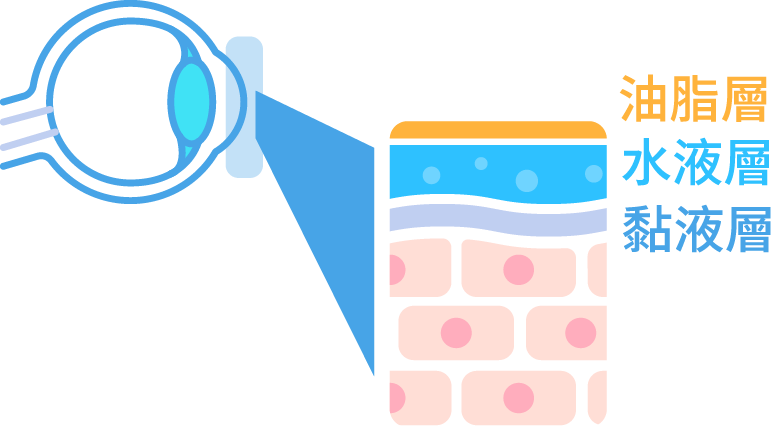
If one of the layers decrease in production, it may cause dry eyes. Eyes may feel dry, have a gritty sensation or stinging.
Types of Dry Eyes
If the lacrimal gland is damaged, degraded or becomes abnormal, the secretion of tear will decrease. Aqueous-deficient dry eye may be caused by ageing, e.g. the elderly and menopausal women (hormonally influenced) produce fewer tears or those with autoimmune diseases.

The dysfunction of the meibomian glands near the eyelashes is the main cause of evaporative dry eye. These glands secrete lipid of the tear film onto the ocular surface, slowing down the evaporation of the aqueous layer of the tear film. When there is an abnormal secretion of the meibomian glands, the tears will lack a lipid layer and water will evaporate rapidly, causing the evaporative dry eye.

Most patients have mixed dry eyes, including both symptoms of insufficient tear secretion and increased tear evaporation rates.
Causes
Aging
The human body's tear secretion function gradually degrades with age, which is one of the main causes of dry eye syndrome.
Hormonal influences
Post-menopausal women are more likely to have dry eyes than men of the same age.
Patients with immune system diseases
Examples include diabetes, thyroid-related diseases, lupus, rheumatoid arthritis and Sjogren’s syndrome.

Prolonged use of electronic products
Blinking less frequently, resulting in tear evaporation.

Long-term contact lens wear
Reduces sensitivity of the corneal surface and deprives the cornea of oxygen, leading to reduced tear secretion and, most likely, dry eyes.

External environment
Dry weather or windy outdoors, indoor air conditioning and heating can reduce humidity and accelerate the evaporation of tears.

Take Medicine
Taking medications such as antihistamines, antidepressants, certain blood pressure medications, and birth control pills increase the risk of dry eye.

Eyelid issues
Severe dry eyes can be caused by abnormal or insufficient blinking reflex or incomplete eyelid closure during sleep.
Cataract treatment/ laser vision correction treatment
The wound is made by cutting through the cornea or cutting the nerve of the cornea, resulting in change of sensitivity of the corneal surface and tear film stability.
Symptoms
Persistent dry eye
Red eye
Itchy eye
Foreign body sensation

Stinging & aching

Burning sensation
Stringy mucus in or around eyes
Sensitivity to light

Eye fatigue
In serious cases, patients will experience eye redness, hyperaemia, keratinisation, corneal abrasion, etc.

Dry eye disease examination method
A variety of tests and measurements with international standards are used to analyse the ocular surface and diagnose dry eye, from the analysis of tear quality to the meibomian gland.
- Testing for the lipid layer of the tear film
- Test for measuring the lipid layer
- Break-up time test for aqueous layer
- Blepharitis
- Tear volume assessment

Management of Dry Eye Syndrome
Intense Pulsed Light
Intense Pulsed Light (IPL) therapy, also known as photorejuvenation therapy, is used at the CUHK Medical Dry Eye Centre with the latest IPL technology to treat patients with meibomian gland dysfunction (MGD)–related dry eye. IPL therapy applies pulses of light to generate a thermal effect that helps to unblock the meibomian glands, restore normal oil secretion, and reduce tear evaporation.
Ophthalmologists may manually press the patient’s eyelids to express blocked oils from the meibomian glands, enhancing the effectiveness of dry eye treatment. During IPL therapy, patients must wear protective goggles, and ophthalmologists carefully adjust the light intensity to minimize risks. A minimum of 3–4 treatment sessions is usually required to achieve optimal results.
Post‑Treatment Care Instructions
On the day of treatment, patients are advised not to drive, although they may resume other normal daily activities. Eyelid hygiene and warm compresses should be reinforced, spicy foods should be avoided, and extra sun protection is required during the week following treatment. IPL therapy is a gentle and painless treatment method, and it is suitable for all patients.
Dry eye syndrome is a chronic condition that often requires long‑term treatment, along with patient cooperation in making lifestyle changes.
Artificial tears
The use of artificial tears can alleviate dry eye symptoms, avoid corneal damage, and keep the surface of the eyeball smooth.
Artificial tears are divided into 3 types:
Drop type: Eye drops have a basic moisturizing effect and are usually used 4 times a day. There are also individually packaged artificial tears. If you have special needs or if you use them more than 4-6 times a day, you can use them according to the doctor's advice. Since they do not contain preservatives, they need to be discarded 24 hours after opening.
Gel type: It is more viscous than the ointment type and has better moisturizing effect. It can prolong the retention time of water. It will slightly blur the vision after use. If you are worried about affecting your work, you can also use it before going to bed, but the problem of blurred vision is lower than that of the ointment type.
Ointment type: The ointment type has the longest effect. After use, you can close your eyes for 5 minutes and rotate your eyes to make the distribution even. Since it will cause short-term blurred vision, it is recommended to use it before going to bed.

iTEAR Autologous Tear Booster
Uses non-invasive vibration technology to stimulate autologous tear secretion through external nasal nerve stimulation. Read more. iTEAR Autologous Tear Booster.
Features:
- Restore your own tear secretion ability
- Clinically proven that after 30 days of use,the native tear secretion level is significantly increased by 56%[1]restore the eye’s natural tear production, relieve dry eye from the root cause, or reduce reliance on artificial eye drops.
- Improve tear film stability
- Clinically proven to help slow down the evaporation of tears after 30 days of use.improve tear film stability (TBUT*+33%)1, soothes symptoms of dry eyes caused by corneal dryness * Tear break up time (TBUT) is a direct measurement method for measuring the stability of the tear film. It refers to the time from a complete blink (the movement of opening and closing the eyes and face) to the appearance of the first dry spot on the tear film.
- Drug-free, preservative-free, all natural
- Recognized by international authoritative organizations
- International Tear Film and Ocular Surface Association[2]and FDA[3]all agree that stimulation of the nasal nerve can help one's own tear secretion.
How to use:
- Just place the vibrating head of iTEAR gently at the junction of the soft and hard bones of the nose, and it will vibrate the nose through a unique vibration frequency, effectively promoting the secretion of tears.
- Use on each alae nasi for 30 seconds, once in the morning and evening
-Change of mean Schirmer score at baseline to day 30 is from 6 to 9.4mm.
-Tear break up time (TBUT) is improved from 5 to 6.7 sec in day 30.
-The mean Schirmer score changed from 6 to 28 mm after stimulation.
2 Jones L et al. Ocul Surf (2017), 15:575-628.
3 De Novo Classification Request For iTEAR100 Neurostimulator. Available at
https://www.accessdata.fda.gov/cdrh_docs/reviews/DEN190026.pdf Accessed on 19 JAN 2022.

Hot compress
Applying warm compresses to the eyes can help prevent dry eye and relieve discomfort caused by the condition. A warm pack or towel at around 40°C can be placed over the eyes for about 10–20 minutes, at least once or twice daily. If time allows, this can be done up to four times a day.

20:20:20 rule
After using electronic products for 20 minutes, rest for 20 seconds, look at the scene 20 feet away, and close your eyes to let tears moisten the surface of the eyeballs.

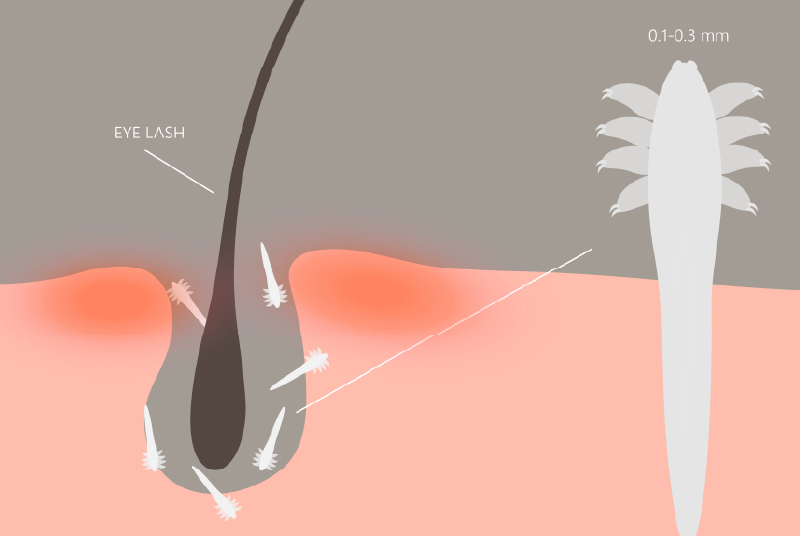
Infestation of eyelashes with mites (ophthalmodermatitis)
Demodex mites often live in the eyelash follicles, and the secretions and excretions they produce can easily cause ophthalmitis. People of any age can be infected, especially those over 70 years old. Because the immune system of older people is weak, they are prone to ophthalmitis. Mites can be transmitted through cosmetics, so girls who often use cosmetics are also more susceptible to infection. Once you suffer from eye dermatitis, it will affect the quality of your tears, resulting in the inability to moisturize the surface of your eyes, leading to dry eyes, excessive secretions, red eyes, foreign body sensation and other discomforts.
Management of Demodex Infestation
♦ Tea tree oil
Using diluted tea tree oil applied to the eyelids requires at least one month of treatment to ensure that both adult mites and their eggs are eliminated. However, it should be noted that tea tree oil may irritate the eyes, and excessive use can cause dryness of the eyes and surrounding skin.
♦ Colored light or red light laser treatment (IPL)
It can penetrate into the pores to eliminate Demodex mites, and compared with tea tree oil, it generally has fewer side effects, making it a relatively new treatment option.
Dry Eye FAQs
What should do if I have dry eyes?
Manage your screen time properly and follow the 20:20:20 rule: Take a 20s break after 20 min of using electronic devices and view from 20ft away. Close your eyes and let the tears moisten the eye surface.
If you wear contact lenses, it is advisable to reduce the amount of time you wear them, for example by removing them immediately after returning home. If the symptoms become severe, you should consult an ophthalmologist.
How can I relieve the discomfort of dry eyes?
- In case of eye discomfort, artificial tears (in preservative-free or contact lens formulations) can be used to temporarily relieve the condition.
- Blink more often to evenly distribute the tears and moisten the eye surface.
- Applying warm compresses to the eyes can help prevent dry eye and relieve discomfort. A warm pack or towel at approximately 40°C can be placed over the eyes for about 10–20 minutes, at least once or twice daily. If time allows, this can be done up to four times a day.
Can I manage dry eye on my own?
Artificial tears, frequent blinking, and warm compresses can help relieve dry eye symptoms and prevent further corneal damage, but they cannot cure dry eye syndrome on their own. To properly manage dry eye, patients should consult an ophthalmologist for treatment options such as IPL (intense pulsed light therapy), medicated eye drops, or punctal plugs.
How long does it take for dry eye syndrome to heal? Will it get better?
IPL (intense pulsed light) therapy usually requires at least 3–4 sessions to achieve the best results. Dry eye syndrome is a chronic condition that often requires long‑term management, along with patient cooperation in making lifestyle changes.
What is Tear Secretion Test (Schirmer's Test)? What is the normal value?
Tear secretion examination is a common examination method in ophthalmology, which is used to detect lesions caused by excessive tear secretion.
A normal person's tear secretion volume in five minutes can reach more than 10mm; if the tear test collects a basic tear volume of less than 5mm in five minutes, it indicates dry eye syndrome.


